From stroke to communication disorders to traumatic brain injuries, researchers at the University of South Carolina are working across several academic disciplines to better understand the workings of the brain and to improve treatments and outcomes for patients.
The university’s efforts are multifaceted, covering multiple conditions and emanating from many schools and colleges. Neuroscience expertise runs throughout USC, including researchers in the Arnold School of Public Health, the School of Medicine Columbia, the College of Arts and Sciences, the Molinaroli College of Engineering and Computing, and the College of Pharmacy.
Along with research that looks at many facets of brain development and disorders, USC is planning to develop a clinical neurological and rehabilitation center. It will become South Carolina's first standalone comprehensive medical facility dedicated entirely to integrated care of patients with brain and nervous system illnesses.
Below is a sampling of USC’s ongoing efforts in the area of neuroscience.
The University of South Carolina is planning to develop a clinical neurological and rehabilitation center that would house the Palmetto State’s first standalone comprehensive medical facility dedicated entirely to integrated care of patients with brain and nervous system illnesses.
USC’s highly specialized center would offer advanced neurological and neurosurgery treatments, as well as neurological rehabilitation for trauma, stroke, cancer and other conditions. The innovative clinical center, concentrating solely on the care of diseases affecting the brain and the nervous system, would be the first of its kind in the Southeast.
The center would provide an opportunity to address the pressing health needs of South Carolinians, while leveraging the broad multidisciplinary clinical, academic and research portfolio from USC.
“As USC expands its efforts to provide the highest quality medical education to South Carolina students and serve the state’s health care needs, building a single location for neurological treatment and rehabilitation is a vital next step,” President Michael D. Amiridis says.
Ana Pocivavsek, a researcher at the School of Medicine Columbia, has received a four-year NIH grant to investigate how poor sleep during critical brain development windows — like pregnancy, childhood and adolescence — affects cognition and mental health.
Pocivavsek and her team aim to uncover the lasting impact of sleep quality on behavioral outcomes and cognitive impairment. Her multidisciplinary approach combines neuroscience, AI and computer science, and is paving the way for new treatments for sleep-related mental health issues and advancing understanding of brain development across the lifespan.
“I study the impact of sleep across the lifespan during windows that are critical to brain development,” says Pocivavsek. “I'm really interested in how disrupted sleep during pregnancy can have an impact on early brain development.”
From the comfort of his couch, a child is able to undergo an electroencephalogram for a study on autism led by Caitlin Hudac, director of USC’s Brain Research Across Development lab. Hudac measures the child's brain’s electrical activity as he repeats different tasks, like watching a video or interacting with another person.
Hudac first took her lab on the road to test children who have rare genetic conditions and couldn’t travel. Now, she hopes to expand the reach of mobile EEG and make research more accessible to all participants.
Mobile EEG testing is a process Hudac has refined since she first took her lab on the road due to pandemic-era restrictions in 2020. At that time, Hudac was a faculty member at the University of Alabama and had grants to study children with rare genetic disorders. The plan had been to fly these families to Tuscaloosa to participate.
“But COVID shuttered that opportunity,” Hudac says. “So, I packed up my EEG equipment, drove around the country and saw more than 55 people in about 90 days.”
This road trip transformed how Hudac, now an associate professor at USC, approaches testing. Some of her participants have rare genetic disorders (specifically GRIN2B, SCN2A or SETBP1) and deal with complex medical symptoms including epilepsy, motor and cognitive delays, and often autism. Hudac found that visiting the families at home makes the testing experience much better for these kids, who benefit from being in their own environment without the stress of travel.
“I can test the same exact brain measure, and the kids are just so much more relaxed when they’re sitting on their own couch with their dog at their feet,” she says.
Today, South Carolina residents with complex brain-related conditions often have to travel out of state for treatment. But it doesn’t have to be this way.
With USC’s plans to build the state’s first clinical neurological and rehabilitation center in downtown Columbia, South Carolinians will be able to get the top-level care they need close to home.
In the video that follows, USC leaders in research and medicine explain why this center is needed and the role it would fill in South Carolina and beyond.
“The idea is to address these issues quickly with new expertise and with a continuum of care under one roof so they can see the neurologist or the neurosurgeon and then also see the physical therapist or the speech therapist right after,” says Stacy Fritz, chief health officer and associate vice president for student health and well-being.
Alessandra Porcu had her sights set on being a forensic detective, analyzing crime scenes for chemical clues. Her colleague Chase Francis once dreamed of becoming an astrophysicist.
Their respective academic journeys led them to new interests and, ultimately, to joining the faculty of USC’s College of Pharmacy, pursuing research aimed at helping people affected by depression, stress and anxiety. That focus is the basis for a developmental research grant from the National Institute of Mental Health shared by the two assistant professors.
Porcu is studying the effects of circadian rhythms, including their effects on administering medications at optimal times of day for maximal efficacy. She also studies how blue light emitted from screen devices affects the adolescent brain.
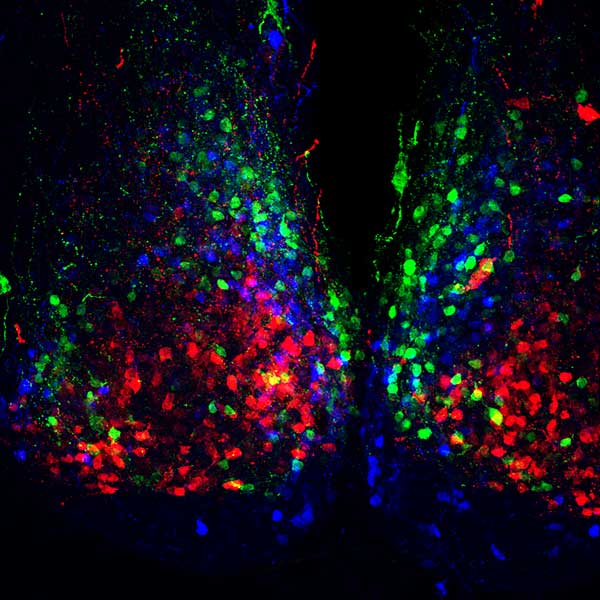
Francis’ research is focused on the nucleus accumbens, a motivation-related area of the brain that is heavily affected in people who have depression.
“We’re trying to find new ways of stimulating the exterior of the brain to affect the nucleus accumbens,” says Francis. “There also are targets that we’re interested in that affect the circuits of the nucleus accumbens and could be the basis for novel therapeutics for depression.”
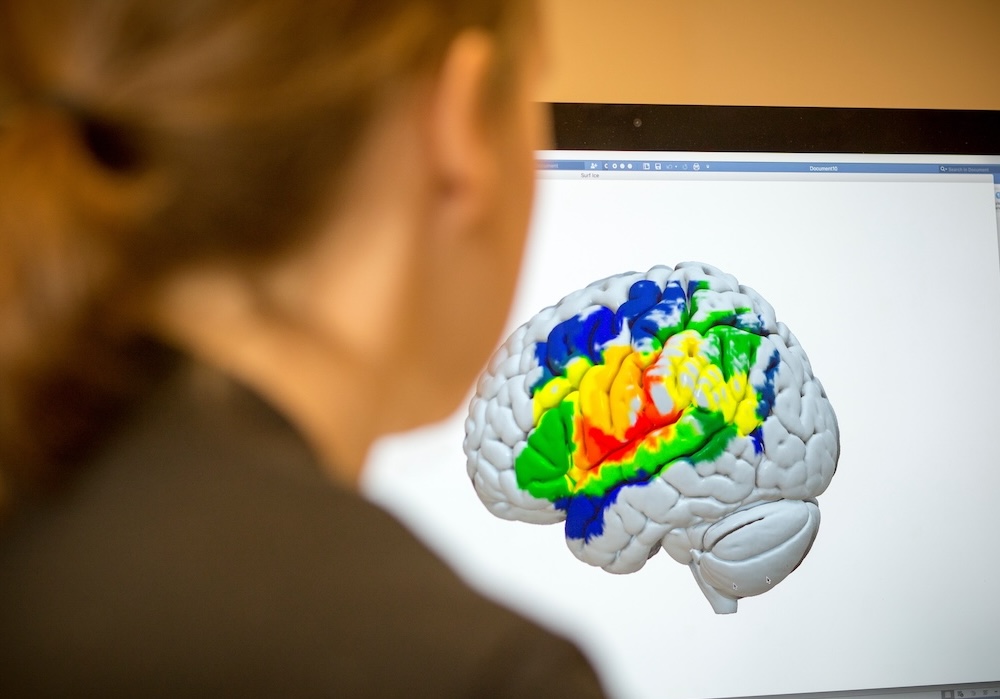
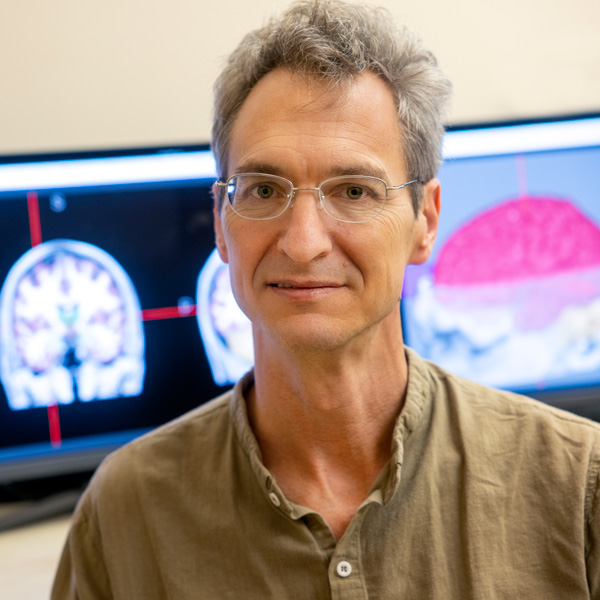
The arrival of two new MRI machines for brain scanning at the University of South Carolina could lead to a better understanding of neurological disorders such as stroke-induced aphasia and dementia.
- One of the scanners, an ultra-high field 7-Tesla, will allow researchers to see brain structure and function with much greater detail and clarity than is possible with the current suite of 3-Tesla scanners.
- The second new scanner will be an extra-large 3-Tesla, matching the power and resolution of current scanners in the university’s brain imaging center but also expanding the population of patients who can be evaluated.
The scanners will be part of USC’s new Brain Health Center, a state-funded initiative to focus physicians and researchers on solving cognitive health problems and reduce disparities in cognitive health care in South Carolina and beyond.“
Our task now as a university is to recruit more scientists like that who can really leverage this new equipment and our Brain Health Center," says Chris Rorden, psychology professor and director of USC's McCausland Brain Imaging Center in support of the university’s neuroscience research portfolio, including projects happening in the Aphasia Lab and the Center for the Study of Aphasia Recovery.
Qun Lu’s quest to develop an effective drug treatment for Alzheimer’s and other neurodegenerative diseases has brought him to the University of South Carolina as the SmartState Endowed Chair in Neurotherapeutics Chemical Biology.
Lu and his research team have developed novel therapeutic molecules that have demonstrated effectiveness in rodent models that mimic Alzheimer’s disease.
The therapeutic compound targets a key signaling cascade in the brain believed to play a critical role in the manifestation of Alzheimer’s and related diseases, including Parkinson’s and amyotrophic lateral sclerosis (ALS), and might also play a role in disorders such as schizophrenia and autism, Lu says.
“We’ve already been issued a U.S. patent, and we’re excited about results we’ve seen in rodent models,” Lu says. “We’re at the stage now where we want to try the molecules on different disease models.”
ABOUT ALZHEIMER'S DRUG RESEARCH
More than 214,000 people were hospitalized for traumatic brain injury in 2020, with more than 69,000 TBI-related deaths reported in 2021, according to the Centers for Disease Control. TBI may lead to short or long-term health problems.
USC biomedical engineering assistant professor Ahmed Alshareef is working to better understand the biomechanics of the human brain during high-severity impacts.
Alshareef’s five-year, $2.6 million project is funded by the National Institute of Neurological Disorders and Stroke and the National Institutes of Health. The multi-institution project is in collaboration with the University of Virginia and Uniformed Services University, and aims to combine to learn more about how the brain deforms from external impacts to the head, which is relevant to automotive crashes, concussions, and military and sports-related blunt impacts.
“If we can measure the relationship between how the head moves and how the brain deforms
during an impact, we can develop tools to mitigate those injuries,” Alshareef says.
“This includes tools that account for different sized heads or brains, and other subject-specific
factors that can lead to different mechanical responses or risk of injury.”