Improving Speech Perception in Cochlear Implant Listeners through Enhanced Electrode-Neuron Interface
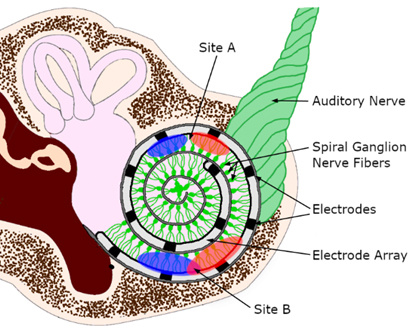
Cochlear implants (CIs) are the most successful neural prosthesis, and they help people
with severe to profound hearing loss access sounds by bypassing the damaged hair cells
in the inner ear and directly stimulating the auditory nerve fibers using an array
of electrodes. The electrical stimulation spreads from each electrode to the surrounding
spiral ganglion nerves (Sites A and B). The quality of these current spreads is impacted
by the quality of interface between CI electrodes and neurons. Limited spread (Site
A) allows for distinct sensations of frequency and speech information, while wider
spread increases the chance of channel interaction (Site B) and complicates differentiation
of sound frequencies allocated to these channels. We combine psychophysical, signal
processing, and neuroimaging methods as diagnostic precursors to assess the CI channel
functionality and develop efficient and selective stimulation strategies tailored
to individual CI listeners. The goal is to maximize the benefits of cochlear implants
and enhance the user's ability to hear and communicate.
Language Development in Children with Cochlear Implants: The Role of Early Linguistic Environments
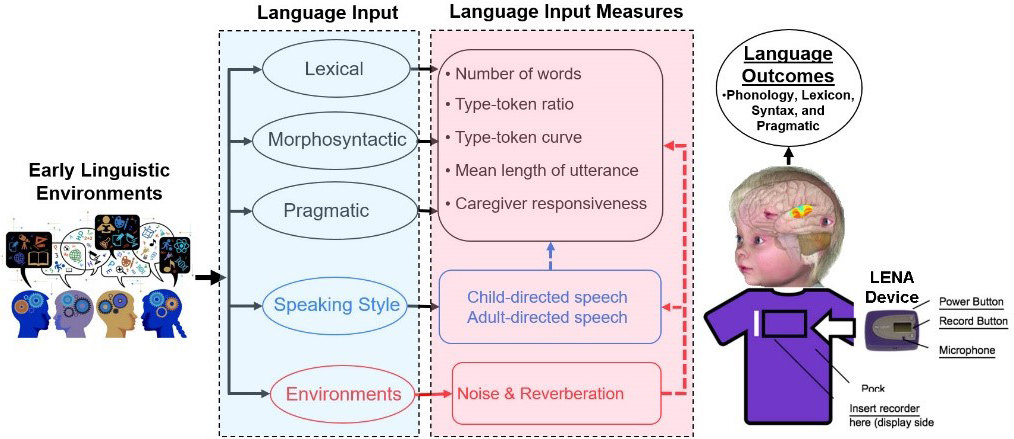
The role of properties of early language input on language outcomes of children with
CIs is not fully understood. We use the Language ENvironment Analysis (LENA) device,
a small, child-safe audio recorder that children wear for a day at a time, to record
and analyze adults’ language input and child vocalization. We use these recordings
to analyze acoustic-phonetic, lexical, morphosyntactic, and pragmatic information,
as well as the effects of caregivers’ speaking styles and the noise and reverberation
in the environment. Our goal is to provide new knowledge for evidence-based early
intervention strategies to clinicians and parents for maximizing the likelihood of
effective oral communication skills in children with CIs.
Consequences of Cochlear Implants for Voice and Speech Production
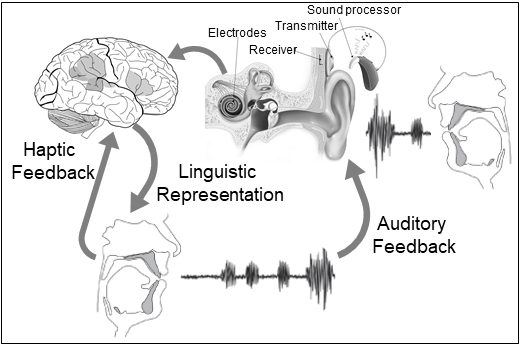
While the primary aim of cochlear implantation is to enhance the overall communication abilities of the recipients, the current evaluation of CI outcomes has predominantly concentrated on the auditory perceptual abilities. However, successful spoken communication necessitates not only efficient auditory perception but also precise speech production. The perception of talkers’ voice and vocal control in CI listeners remain poorly understood. We combine behavioral, electrophysiological (EEG), and functional neuroimaging (fNIRS) techniques for studying the ability of CI listeners in vocalization and perception of voice. The findings will provide important information on whether and to what extent CI impacts and restores the sensorimotor pathways in CI patients and how to improve diagnosis and targeted treatment for enhanced vocal control in CI patients.
Neurocognitive Mechanisms Linking Hearing Impairment, Social Isolation, and Cognitive Decline
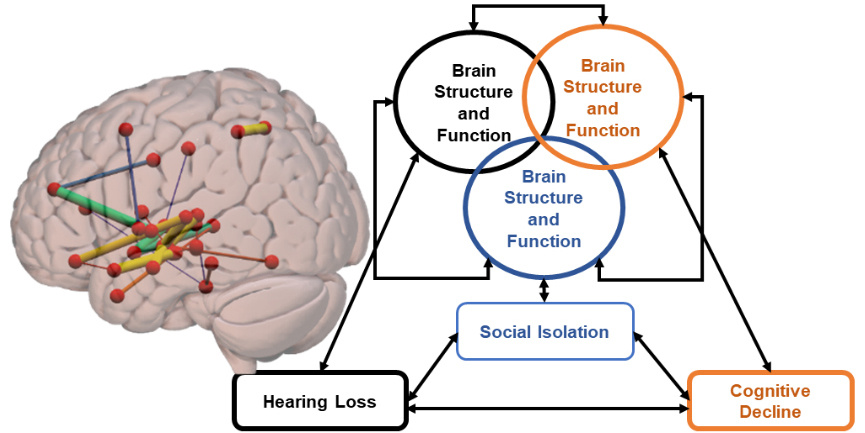
In collaboration with the USC Aging Brain Cohort (ABC) and Aging Gracefully Lab, we investigate the relationship between hearing loss, social isolation, and cognitive decline in adults. We use beh avioral and neural assessments, including functional and structural connectivity measures obtained from DTI and MRI, to study a vicious cycle created by hearing loss, social isolation, and cognitive decline, in which each factor may contribute to and exacerbate others. The knowledge gained will be used to develop effective interventions and treatments to promote hearing, social interaction, and cognitive functions in older adults, ultimately improving their health, well-being, and quality of life by breaking this vicious cycle.
Collaborations
Coordinator, Beth McCall, AuD, CCC-A
Department of Communication Sciences and Disorders
University of South Carolina
Director, Dr. Jean Neils-Strunjas
Department of Communication Sciences and Disorders
University of South Carolina
Director, Dr. Julius Fridriksson
Department of Communication Sciences and Disorders
University of South Carolina
Director, Dr. Rutvik Desai
Department of Psychology
University of South Carolina
Director, Dr. Julie Arenberg
Massachusetts Ear and Eye Infirmary
Department of Otolaryngology, Harvard Medical School
Director, Dr. Laura Dilley
Department of Communicative Sciences and Disorders
Michigan State University
Department of Speech, Language and Hearing Sciences
University of Connecticut